Background: Conventional risk factors for inferior outcomes in polycythemia vera (PV) include elevated hematocrit, white blood cell (WBC) count, age, and abnormal karyotype. Weight loss adversely impacts survival in cancer patients. JAK2 myeloproliferative neoplasms (MPN) upregulate tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), and IL-8 and induce decreased leptin levels leading to weight loss. The impact of weight loss in PV patients receiving best supportive care (i.e. frontline hydroxyurea [HU] therapy, phlebotomy) on overall survival (OS) is largely unknown. In this study, we seek to investigate: (1) differential effect on survival for weight loss, and (2) variables with predictive value for weight loss among JAK2 inhibitor-naïve PV patients.
Methods: After IRB approval, 46 patients at the Michael E. DeBakey VA Medical Center diagnosed with PV between 2000 and 2016 were selected for analysis. Our outcome of interest was OS among PV patients exhibiting weight loss versus patients who maintained, gained weight or had minor weight loss. To objectively estimate weight changes overtime, the difference between baseline BMI [BMI-B] at the time of diagnosis and BMI at last follow-up (BMI-L) was obtained for each patient. Survival analysis was performed for PV patients exhibiting more than 10% weight loss (>10%) versus all other patients (less than 10% loss, stable and increased weight) (<10%) over time. Kaplan-Meier (KM) method was used to determine OS. Cox regression model was performed to assess independent role of different variables including age, blood cell counts and ferritin level Statistical analysis was performed using SAS software.
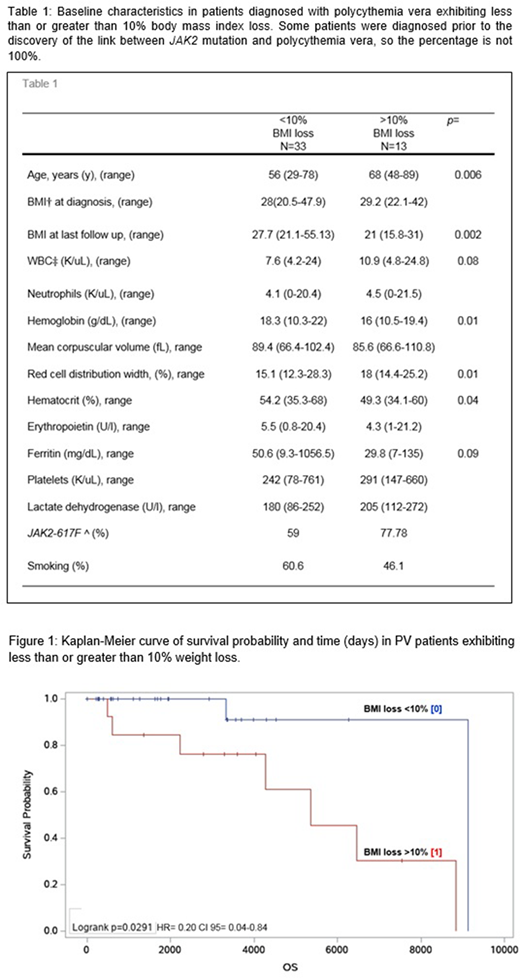
Results: Median BMI loss was 10% (0.03-36.72%); 33/46 (71.7%) and 13/46 (28.2%) patients developed <10% and >10% BMI loss, respectively. Baseline characteristics are summarized in Table 1. Median BMI at last follow up was 21 for PV patients exhibiting >10% BMI loss and 27.7 for PV patients exhibiting <10% BMI loss (p<0.01). Median age was higher among patients exhibiting >10% BMI loss (68 vs 56 y, respectively, p=0.006). A non-significant clinical trend for higher WBC was observed among patients losing >10% BMI (10.9 vs 7.6 K/uL, p=0.08). Median Hemoglobin (Hb), hematocrit (Hct) and ferritin were intriguingly lower in the >10% loss group at 16 vs 18.3 g/dL (p=0.01), 49.3 vs 54.2% (p=0.04) and 29.8 vs 50.6 ng/mL (p=0.09) respectively, while median RDW was higher at 18 vs 15.1% (p=0.01). OS was 9125 days vs 5364 days, in patients with <10% and >10% BMI loss, respectively (p=0.02, HR=0.20; CI 95% 0.04-0.84) (Figure 1). On multivariate analysis, age (hazard ratio [HR], 1.34; p<0.02) and WBC count (HR, 1.57; p<0.01), were predictive of OS.
Conclusions: A subgroup of PV patients exhibit progressive weight loss. Over 10% BMI reduction is associated with decreased survival, suggesting that "early weight loss" is an independent clinical variable that predicts high risk PV. While a larger study is needed to validate this observation, this small study highlights the role of leukocytosis, advanced age and weight loss in PV. Confirmation of the observations reported here could unveil an important role for pharmacologic and/or dietary interventions to improve survival among high-risk PV patients.
Rivero:agios: Membership on an entity's Board of Directors or advisory committees; celgene: Membership on an entity's Board of Directors or advisory committees; Incyte: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal